 Happy #WorldDiabetesDay to you! This year’s theme is Family and Diabetes. While the day (and the month) is more aimed at raising awareness of the undiagnosed condition and family members looking out for the signs of diabetes in partners, parents, siblings etc., my day will reflect on my family and how thankful they make me.
Happy #WorldDiabetesDay to you! This year’s theme is Family and Diabetes. While the day (and the month) is more aimed at raising awareness of the undiagnosed condition and family members looking out for the signs of diabetes in partners, parents, siblings etc., my day will reflect on my family and how thankful they make me.
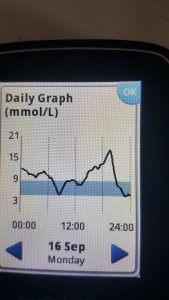
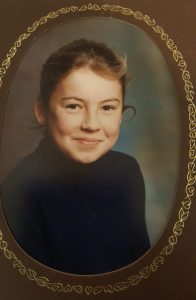
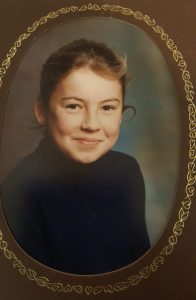
I was diagnosed with type 1 at the age of nine (there I am, just post-diagnosis on the right). Since then, diabetes care has come along in leaps and bounds. In those days, you used syringes made of glass, tested your urine and not your blood and relied heavily on your body and not a machine to tell you what was wrong. (Ah, the young yins! Don’t know they’re born…)
As a nine-year-old weeping copiously at the prospect of no sweeties or birthday cake again ever, I wasn’t 100 percent au fait with what was now going on with my body. I scared the living daylights out of my parents several times by fainting first thing in the morning. The most memorable time when I jumped up on the kitchen window ledge to let our pet cat in and fell off it. Onto a stone floor.
Bite me…
As biting my tongue often went along with fainting, my dad would try to stop me by inserting his own hand. I bit that instead.
Still, my parents were a game pair—happy to downplay the condition so I never felt disadvantaged. It took me until my 20s to realise I had a chronic illness. Duh, I know, but diabetes never felt that way to me growing up. My mum’s favourite cry was, “Have you got your Dextrosol?” whenever I left the house. (Again, the young yins. Not having to use Dextrosol for their hypos.) But other than that, they never mentioned it as a limiting factor or felt I could not do anything because of the diabetes. Fair enough, I announced no plans to be an athlete, truck driver or pilot, but they waved me off to a university in another country, a kibbutz, solo living and more without fuss.
Whenever I called home or visited, questions concentrated on my job, my personal life, what I was doing… diabetes never took centre stage.
Then, as I got older they generously funded a pump for me for a few years. When it gave up the ghost, I decided against further funding as I didn’t want to take any more of their money. They would have handed it over gladly. And still would, even though there are no longer two of them…
Ah, the mood swings…
Any family member of someone who has diabetes will raise a wry eyebrow if you talk about the mood swings. Figures, after all, that if you have a chronic illness tiredness is a frequent friend of the not very nice sort. It makes you sullen and snappy. Who better to take that out on than your nearest and dearest?
Then, there are the ‘hypo experts’; mums and partners who can tell you are hypo before it strikes you the excessive yawning is more to do with plunging blood sugar levels than a late night the day before. Grr. Double grr because they are almost always right.
I have my own little circle of mood bearers—once upon a time my mum, dad and sisters. (Still my poor old mum to some extent). Nowadays, my husband. He’s awfully good at spotting hypos. Awfully brilliant at lots of other things too. Running upstairs to bring me supplies when I run out of needles and other equipment. Keeping me in jelly baby supplies. Factoring in blood glucose checking stops whenever we are out and about. Finding me ice-cold water when high blood sugars kick in. Accepting that I am terrifically rubbish at late nights, which means we do not go out that much. (Tip—I organise a lot of things for a Sunday afternoon.) Checking restaurants to see if they offer low-carb options before booking them.
Diabetes does not come alone. Yes, it includes tiredness and a whole slew of other complications you do your best to avoid. But if it takes a village to raise a child, it takes warm, supportive, kind and patient folks to nurture a diabetic.
Here’s to them all—my family. Thank you thank you thank you.





 Happy #WorldDiabetesDay to you! This year’s theme is Family and Diabetes. While the day (and the month) is more aimed at raising awareness of the undiagnosed condition and family members looking out for the signs of diabetes in partners, parents, siblings etc., my day will reflect on my family and how thankful they make me.
Happy #WorldDiabetesDay to you! This year’s theme is Family and Diabetes. While the day (and the month) is more aimed at raising awareness of the undiagnosed condition and family members looking out for the signs of diabetes in partners, parents, siblings etc., my day will reflect on my family and how thankful they make me. Maybe it’s the Extinction Rebellion folks gluing their hands to pavements, disrupting flights and parking their uncooperative crusty* posteriors on roads throughout central London.
Maybe it’s the Extinction Rebellion folks gluing their hands to pavements, disrupting flights and parking their uncooperative crusty* posteriors on roads throughout central London.